According to the American Heart Association, about 356,000 Sudden Cardiac Arrest (SCA) cases happen outside of the hospital in the U.S., and about 90% of these cases result in death.
The American Heart Association has developed a chain of survival that includes six crucial steps to saving someone’s life.
1) Activation of Emergency Response
2) Early CPR
3) Rapid Defibrillation
4) Advanced Resuscitation by Emergency Medical Services
5) Post Cardiac Arrest Care
6) Recovery
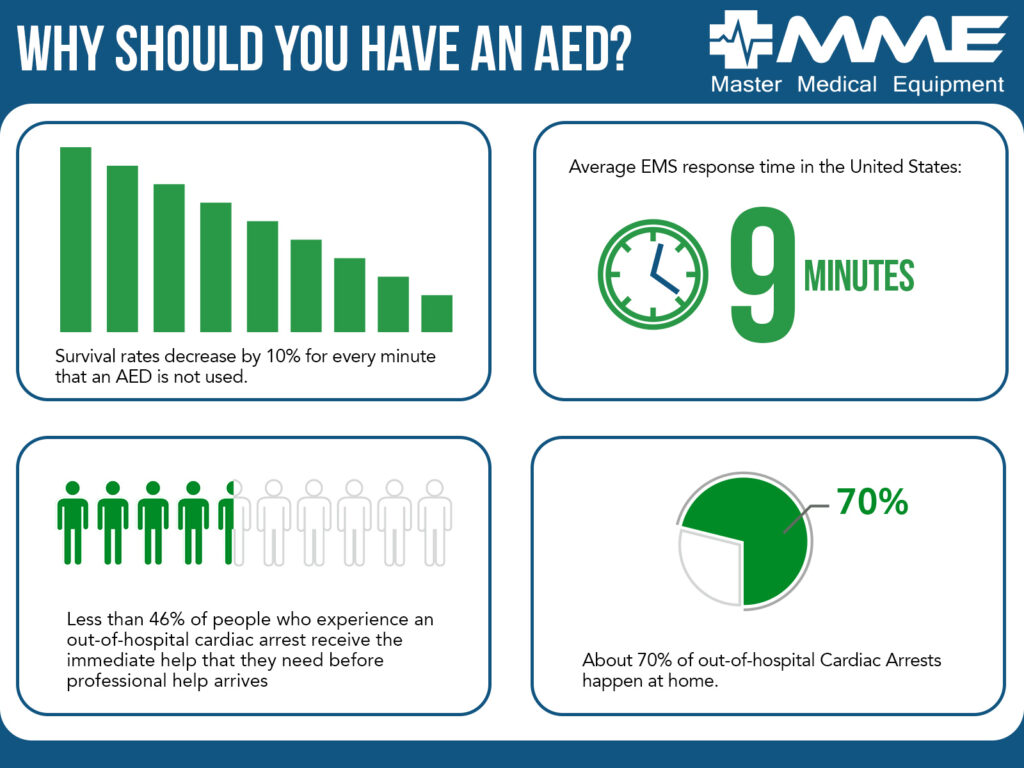
Immediate Cardiopulmonary Resuscitation, or CPR, is crucial to saving a life. When someone experiences SCA, their heart stops beating, keeping oxygenated blood from moving throughout the body, including the heart, lungs, and brain. Each minute after the SCA without oxygen flow through the body decreases survival odds by approximately 10%.
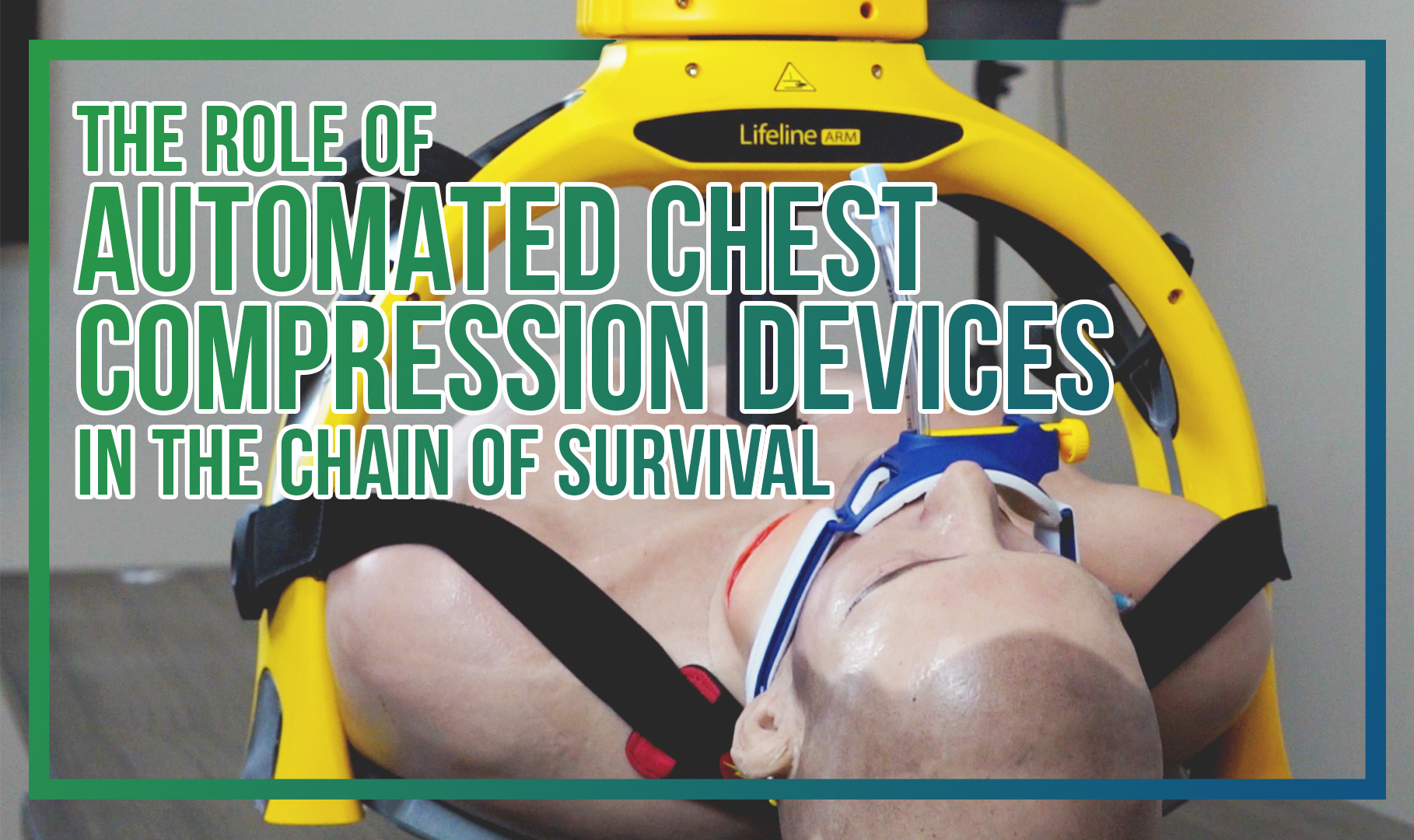
The second step in the Chain of Survival, Early CPR, will usually be performed manually before a defibrillating shock is administered. Although they can be used before administering a shock, Automated Compression Devices can play a role during step four, Advanced Resuscitation by EMS personnel. Advanced resuscitation by EMS often involves CPR while transporting a patient on a stretcher or in an ambulance for an extended time before getting to a hospital.
CPR involves two steps: giving chest compressions and administering breaths. Chest compressions are the most essential part of CPR, and we’ll focus on them here. When performed at the proper depth and rate, chest compressions help keep the blood flowing in a victim’s body and immediately improve survival chances.
A retrospective study analyzed a data set from one million EMS incidents in 2018, specifically looking at the impact of automated compression devices in out-of-hospital cardiac arrests.
These chest compression devices are an efficient tool to free up hands to continue a rescue. These devices have seen the most impact in teams of 2. Often when it comes to manual chest compressions, healthcare professionals will have to rotate to rest to provide the best compressions possible. After 10-20 minutes, fatigue wears down rescuers and, consequently, the quality of compressions.¹
When performed correctly, chest compressions are very physically demanding on the caregiver. Fatigue sets in for even the most experienced paramedics and first responders, who need to rotate every two minutes during extended periods of CPR. Fatigue leads to sub-optimal compressions, which can have a very detrimental impact on the victim’s already-low survival odds.
Why use a mechanical compression device?
 In an effort to save more lives, reduce the strain on their paramedics, and free up a pair of hands on a rescue, many large and small EMS companies began integrating automatic CPR into their protocols in 2022. One example of an Automated Chest Compression device is the Lifeline ARM, which retails at approximately half the cost of the leading competitor.
In an effort to save more lives, reduce the strain on their paramedics, and free up a pair of hands on a rescue, many large and small EMS companies began integrating automatic CPR into their protocols in 2022. One example of an Automated Chest Compression device is the Lifeline ARM, which retails at approximately half the cost of the leading competitor.
In order to ensure quality compression depth and rate, the Lifeline ARM’s software-controlled motor algorithm compensates for variability in chest resistance. This allows rescuers to confidently administer CPR without risking poor-quality compressions.
While this article focuses on chest compressions, another element of CPR is pausing for resuscitation breaths. The device can chirp and flash an LED light when pausing for breaths, alerting the rescuer. Not all practices include breath pauses in their quality CPR protocol, but the ARM lets you switch between “breath” or “no breath” based on your local protocol.
Automated compression devices like the ARM can fit around the patient on most stretchers, allowing quality compressions while transporting the patient and in transit. The ARM’s rugged and lasting battery provides consistent compressions over a long time, and the unit can continue to charge and run on AC power while in the vehicle. Batteries are hot-swappable and can be inserted in multiple orientations for tactical battery reloads with almost no downtime.
Quality compressions save lives, and extended manual compressions lead to a decrease in quality. Chest compression devices lead to less downtime, reliable, smart compressions, and more lives saved.
Have any questions about the Defibtech ARM? Our team is here to provide an answer! To learn about our best price or bulk discounts, request a quote here. Or contact us today to speak to our friendly and knowledgeable team at 866.417.2546 or salessupport@mmemed.com. We can’t wait to save lives together!
¹-Kłosiewicz T, Puślecki M, Zalewski R, Sip M, Perek B. The impact of automatic chest compression devices in out-of-hospital cardiac arrest. J Thorac Dis. 2020 May;12(5):2220-2227. DOI: 10.21037/jtd.2020.04.25. PMID: 32642127; PMCID: PMC7330409.


 Commotio Cordis is very rare — in fact, just over 200 cases have been reported to the U.S. Commotio Cordis registry since the mid-1990s. It’s a condition where an impact to the upper portion of the chest at a specific instance during the heartbeat can disrupt the heart, causing a Sudden Cardiac Arrest. This condition is much less common than a normal SCA, but all forms of Cardiac Arrest require CPR and defibrillation equipment. Otherwise, life could be at risk before the ambulance arrives.
Commotio Cordis is very rare — in fact, just over 200 cases have been reported to the U.S. Commotio Cordis registry since the mid-1990s. It’s a condition where an impact to the upper portion of the chest at a specific instance during the heartbeat can disrupt the heart, causing a Sudden Cardiac Arrest. This condition is much less common than a normal SCA, but all forms of Cardiac Arrest require CPR and defibrillation equipment. Otherwise, life could be at risk before the ambulance arrives.


 “The median chest compression depth using manual CC[Chest Compressions], CPRMeter, and LifeLine ARM varied and amounted to 40 (38–45) vs. 45 (40–50) vs. 51 (50–52) mm, respectively (p = 0.002). The median chest compression rate was 109 (IQR; 102–131) compressions per minute (CPM) for manual CC, 107 (105–127) CPM for CPRMeter, and 102 (101–102) CPM for LifeLine ARM (p = 0.027). The percentage of correct chest recoil was the highest for LifeLine ARM — 100% (95–100), 80% (60–90) in the CPRMeter group, and the lowest for manual CC — 29% (26–48).”
“The median chest compression depth using manual CC[Chest Compressions], CPRMeter, and LifeLine ARM varied and amounted to 40 (38–45) vs. 45 (40–50) vs. 51 (50–52) mm, respectively (p = 0.002). The median chest compression rate was 109 (IQR; 102–131) compressions per minute (CPM) for manual CC, 107 (105–127) CPM for CPRMeter, and 102 (101–102) CPM for LifeLine ARM (p = 0.027). The percentage of correct chest recoil was the highest for LifeLine ARM — 100% (95–100), 80% (60–90) in the CPRMeter group, and the lowest for manual CC — 29% (26–48).” 









 Moving to the mounting bracket, two tabs click into the device for secure placement and can release with the push of a button. The mount is spring-loaded and can rotate according to what orientation you want the device to mount on.
Moving to the mounting bracket, two tabs click into the device for secure placement and can release with the push of a button. The mount is spring-loaded and can rotate according to what orientation you want the device to mount on.
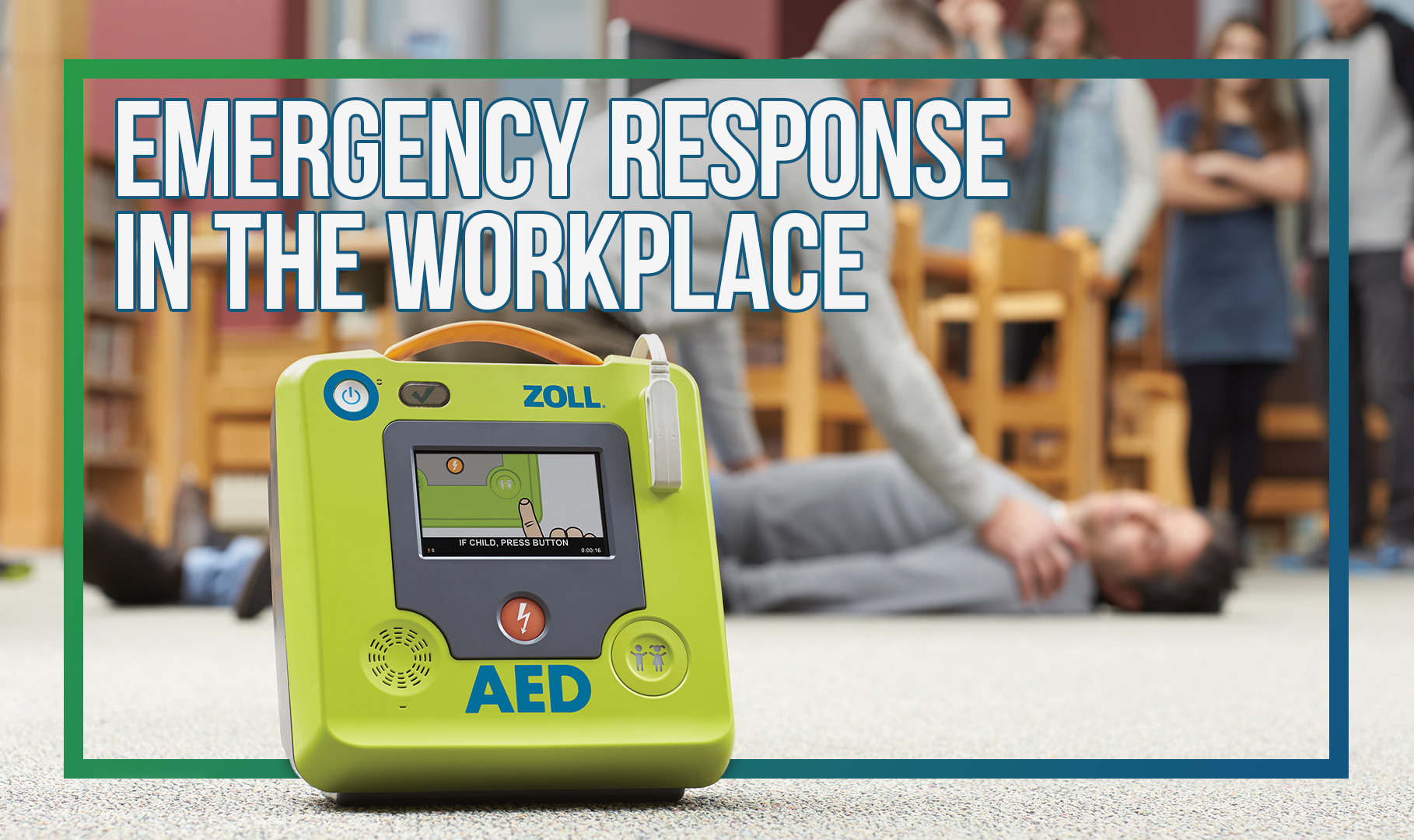


 In an effort to increase workplace safety and preparedness, we are offering a limited-time
In an effort to increase workplace safety and preparedness, we are offering a limited-time 
 for your biomed technician. We also recommend the
for your biomed technician. We also recommend the